Vanderbilt University Medical Center nephrologist and Associate Professor of Medicine Dr. William H. Fissell IV, is making major progress on a first-of-its kind device to free kidney patients from dialysis. He is building an implantable artificial kidney with microchip filters and living kidney cells that will be powered by a patient’s own heart.
We are creating a bio-hybrid device that can mimic a kidney to remove enough waste products, salt and water to keep a patient off dialysis,” said Fissell.
Nanotchnology
The key to the device is a microchip.
“It’s called silicon nanotechnology. It uses the same processes that were developed by the microelectronics industry for computers,” said Fissell.
The chips are affordable, precise and make ideal filters. Fissell and his team are designing each pore in the filter one by one based on what they want that pore to do. Each device will hold roughly fifteen microchips layered on top of each other.
But the microchips have another essential role beyond filtering.
“They’re also the scaffold in which living kidney cells will rest,” said Fissell.
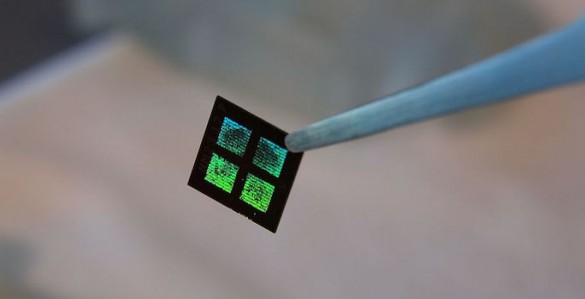
An example of the microchip filter being used inside Fissell's artificial kidney. (Vanderbilt University)
Living kidney cells
Fissell and his team use live kidney cells that will grow on and around the microchip filters. The goal is for these cells to mimic the natural actions of the kidney.
“We can leverage Mother Nature’s 60 million years of research and development and use kidney cells that fortunately for us grow well in the lab dish, and grow them into a bioreactor of living cells that will be the only ‘Santa Claus’ membrane in the world: the only membrane that will know which chemicals have been naughty and which have been nice. Then they can reabsorb the nutrients your body needs and discard the wastes your body desperately wants to get rid of,” said Fissell.
Avoiding organ rejection
Because this bio-hybrid device sits out of reach from the body’s immune response, it is protected from rejection.
“The issue is not one of immune compliance, of matching, like it is with an organ transplant,” said Fissell.
How it works
The device operates naturally with a patient’s blood flow.
“Our challenge is to take blood in a blood vessel and push it through the device. We must transform that unsteady pulsating blood flow in the arteries and move it through an artificial device without clotting or damage.”
Fluid dynamics
And that’s where Vanderbilt biomedical engineer Amanda Buck comes in. Buck is using fluid dynamics to see if there are certain regions in the device that might cause clotting.
“It’s fun to go in and work in a field that I love, fluid mechanics, and get to see it help somebody,” said Buck.
She uses computer models to refine the shape of the channels for the smoothest blood flow. Then they rapidly prototype the new design using 3-D printing and test it to make the blood flow as smoothly as possible.
Vanderbilt biomedical engineer Amanda Buck is using fluid dynamics to see if there are certain regions in the device that might cause clotting.
Future human trials
Fissell says he has a long list of dialysis patients eager to join a future human trial. Pilot studies of the silicon filters could start in patients by the end of 2017.
“My patients are absolutely my heroes,” said Fissell. “They come back again and again and they accept a crushing burden of illness because they want to live. And they’re willing to put all of that at risk for the sake of another patient.”
Federal investment
The National Institutes of Health awarded a four-year, $6 million grant to Fissell and his research partner Shuvo Roy from the University of California at San Francisco. The two investigators are longtime collaborators on this research. In 2003, the kidney project attracted its first NIH funding, and in 2012 the Food and Drug Administration selected the project for a fast-track approval program. The work is supported by NIH grant 1U01EB021214-01.
The National Kidney Foundation reports that in 2012, Federal Medicare dollars paid more than $87 billion caring for kidney disease patients (not including prescription medications).
Desperate need
Transplant of a human kidney is the best treatment for kidney failure, but donor kidneys are in short supply. According to the U.S. Organ Procurement and Transplantation Network, although more than 100,000 patients in the United States are on the waiting list for a kidney transplant, last year only 17,108 received one.
In all, the National Kidney Foundation says more than 460,000 Americans have end-stage renal disease and every day, 13 people die waiting for a kidney.